In the quiet hours of the morning, as the world still slumbers, many rise to an unwelcome ritual. The first steps out of bed become a testament to endurance, a sharp reminder of the invisible struggle etched within the fibers of their feet. This is the daily reality for those battling plantar fasciitis, a condition where every step is a negotiation with pain. Amidst the myriad of treatments and advice, one tool stands out for its clarity and precision in guiding sufferers towards relief: the Plantar Fasciitis MRI scan.
Understanding Plantar Fasciitis
Plantar fasciitis is a common foot condition that causes pain and discomfort in the heel area. The plantar fascia is a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes. It acts as a shock absorber and supports the arch of the foot.
When the plantar fascia becomes irritated or inflamed, it can lead to heel pain, often described as a sharp, stabbing sensation. Plantar fasciitis can also affect the fat pad in the heel, causing pain and tenderness. In some cases, plantar fibromatosis, the development of fibrous nodules in the plantar fascia, can contribute to heel pain as well.
Symptoms of Plantar Fasciitis
The hallmark symptom of plantar fasciitis is heel pain, which is typically worse in the morning or after periods of rest, such as taking the first steps after waking up. The pain is often localized to the bottom of the foot, near the heel, but it can also radiate along the arch area.
Individuals with plantar fasciitis often experience increased pain after standing or walking for prolonged periods, or engaging in activities that put stress on the plantar fascia, such as running or jumping. The pain can range from mild to severe and may interfere with daily activities, affecting the individual’s quality of life.

Causes of Plantar Fasciitis
Plantar fasciitis can have several causes, and the exact mechanism is not always clear. However, certain risk factors can increase the likelihood of developing this condition. Repetitive strain on the plantar fascia, such as from excessive running or walking, can lead to inflammation and heel pain. Foot arch problems, such as flat feet or high arches, can also contribute to plantar fasciitis.
Additionally, obesity, tight calf muscles, and wearing shoes with inadequate support, such as high heels or worn-out athletic shoes, can increase the risk of developing plantar fasciitis. In some cases, plantar fasciitis may be associated with other foot conditions, such as Achilles tendonitis or plantar fibromatosis.
The diagnosis of plantar fasciitis is usually made through a physical examination, where the doctor will assess the symptoms, perform manual tests, and evaluate the range of motion of the foot and ankle. Imaging tests, such as X-rays, ultrasound, or MRI scans, may be ordered to confirm the diagnosis and rule out other potential causes of heel pain.
Why MRI?
MRI is preferred for imaging the foot and ankle because it provides detailed images of the soft tissues, such as the plantar fascia, ligaments, and tendons. Unlike X-rays, which primarily show bony structures, MRI scans allow for the visualization of abnormalities in the soft tissue, such as inflammation, edema, or rupture of the plantar fascia.
During an MRI scan, the magnetic resonance technology generates high-resolution images by measuring the signal intensity of the different tissues in the foot. Abnormalities, such as inflammation or swelling in the plantar fascia, can appear as areas of high signal intensity, indicating potential plantar fasciitis.
On the other hand, normal plantar fascia will show low signal intensity, suggesting the absence of inflammation or other abnormalities. This ability to differentiate between normal and abnormal signal intensities makes MRI a valuable tool for the diagnosis of plantar fasciitis.
What does an MRI show for Plantar Fasciitis?
An MRI scan for plantar fasciitis can reveal important information about the condition of the plantar fascia and surrounding soft tissue structures. Severe plantar fasciitis MRI images may show thickening, inflammation, or rupture of the plantar fascia. These images also provide insights into the presence of swelling or edema in the soft tissue, which is indicative of plantar fasciitis.
The radiologist will analyze the MRI plantar fascia images and look for abnormalities, such as high signal intensity, inflammation, or swelling of the plantar fascia. These findings, along with clinical history and physical examination, confirm the diagnosis of plantar fasciitis.
Additionally, the radiologist can identify other differential diagnoses, such as abnormalities of the fat pad, stress fractures, or tendon issues, which may present similar symptoms. The radiology report will provide detailed interpretations of the MRI scan, aiding healthcare providers in developing the most appropriate treatment plan for plantar fasciitis.

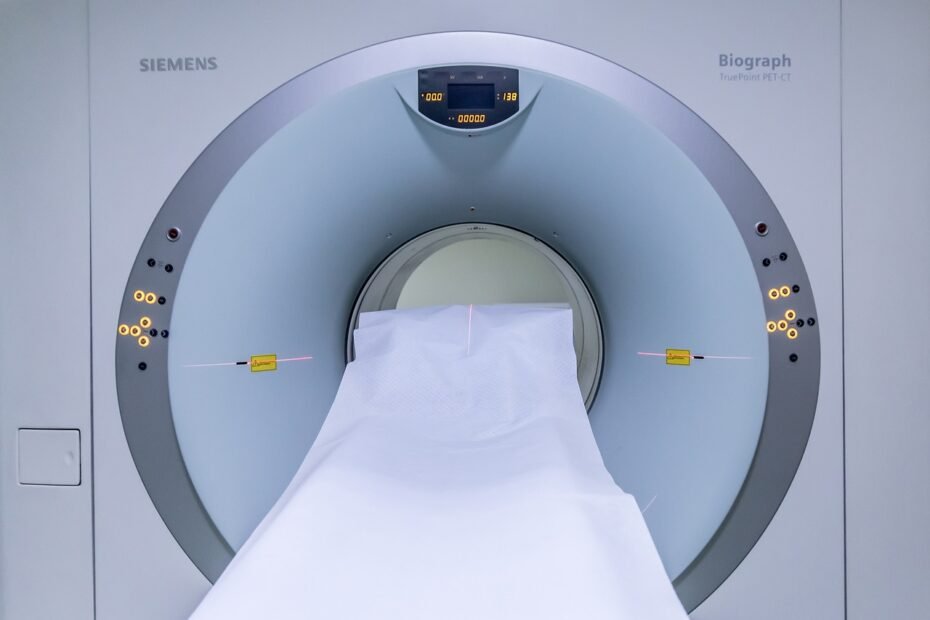
The Process of getting an MRI Scan
If your healthcare provider recommends an MRI scan for plantar fasciitis, you may be wondering what to expect during the process. The first step is to schedule the appointment with an imaging facility that offers MRI services. Prior to the scan, be sure to inform the facility of any health conditions, allergies, or previous surgeries you have had. They may provide specific instructions, such as fasting before the scan or avoiding certain medications. It’s recommended to wear comfortable clothing for the scan, and, if necessary, you may receive a contrast dye for enhanced imaging.
Preparing for an MRI Scan
Before the MRI scan, it’s crucial to prepare properly to ensure the best imaging results. The healthcare facility will provide you with specific instructions, tailored to the plantar fasciitis scan protocol. These instructions may include fasting for a few hours before the scan, especially if a contrast dye is being used.
Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), might need to be avoided prior to the scan, as they can affect the imaging results. Inform the facility of any metal implants, such as joint replacements or pacemakers, as these might interfere with the MRI scan.
What to Expect during the Scan
During the MRI scan, you will lie down on a table that slides into the cylindrical MRI machine. It’s important to remain still during the scan to avoid motion artifacts, which can affect the quality of the images. The machine will produce loud knocking or tapping noises during the scanning process, but don’t worry, these sounds are normal. Earplugs or headphones may be provided to help block out the noise and make the experience more comfortable.
The technologist will monitor the scan from an adjacent room, and you will be able to communicate with them via an intercom system. The scan usually takes around 30-60 minutes, depending on the area of the foot being imaged.
Reading an MRI Scan
After the scan, the MRI images will be interpreted by a radiologist, who is a specialized doctor trained in reading and analyzing imaging studies. The radiologist will carefully examine the plantar fasciitis MRI images to identify any abnormalities related to plantar fasciitis, such as high signal intensity, inflammation, or thickening of the plantar fascia.
They will also evaluate the surrounding soft tissue, fat pad, ligaments, tendons, and other structures of the foot for any secondary findings or differential diagnoses.
The radiology report will provide a detailed analysis of the MRI scan, including descriptions of the abnormalities, the severity of inflammation or swelling, and the presence of any additional foot conditions. This information, combined with the clinical history, physical examination, and other diagnostic tests, will guide healthcare providers in determining the most appropriate treatment plan for plantar fasciitis.
The radiology report may also recommend further imaging studies or consultations with other specialists, if necessary, for a comprehensive evaluation of the condition.

MRI Scan vs Other Imaging Techniques
While MRI scans are highly effective for imaging the foot and ankle, it’s important to understand the differences between MRI and other imaging techniques, such as radiographs (X-rays) and ultrasound. X-rays are primarily used to evaluate bony structures, such as stress fractures or calcaneal abnormalities. However, X-rays have limited visualization of soft tissue abnormalities, such as plantar fasciitis.
Ultrasound imaging, on the other hand, provides valuable information about tendons, ligaments, and soft tissue inflammation associated with plantar fasciitis, but it may not offer the same level of detailed soft tissue imaging as an MRI scan.
X-Ray Examination
X-rays, also known as radiographs, are commonly used in the initial evaluation of foot pain, including heel pain. They are a quick and accessible imaging technique that can help rule out certain conditions, such as calcaneal crescent, stress fractures, or osteoarthritis.
X-rays allow healthcare providers to assess the bony structures of the foot, such as the calcaneus (heel bone), for any abnormalities or signs of damage. However, X-rays have limitations when it comes to visualizing soft tissue abnormalities, such as inflammation of the plantar fascia. Therefore, for a comprehensive diagnosis of plantar fasciitis, additional imaging techniques, such as MRI, may be necessary.
Ultrasound Imaging
Ultrasound imaging is another imaging modality used for the evaluation of plantar fasciitis. It utilizes high-frequency sound waves to create images of the soft tissue structures in the foot, including the plantar fascia, tendons, and ligaments.
Ultrasound imaging can provide valuable information about the soft tissue inflammation and swelling associated with plantar fasciitis. It allows for real-time visualization of the plantar fascia, enabling the radiologist or clinician to perform dynamic imaging, assess the range of motion, and identify tenderness in the affected area.
However, ultrasound imaging may not offer the same level of detailed soft tissue imaging as an MRI scan, which makes MRI the preferred imaging modality for diagnosing plantar fasciitis and assessing the extent of the condition.
MRI Scans
MRI scans are considered the gold standard for imaging soft tissue abnormalities, such as plantar fasciitis. They provide high-resolution images that can reveal the signal intensity, edema, inflammation, or lesions of the plantar fascia and other soft tissue structures in the foot.
The ability to differentiate between normal and abnormal signal intensity enables radiologists to accurately diagnose plantar fasciitis. MRI scans also allow for the detection of other foot conditions that may mimic plantar fasciitis symptoms, such as stress fractures, tendon abnormalities, or bursa inflammation.
The comprehensive visual assessment provided by MRI scans assists healthcare providers in developing an effective treatment plan for plantar fasciitis.

Misdiagnosis and Differential Diagnosis
Misdiagnosis of plantar fasciitis can occur, as the symptoms can overlap with other foot conditions. Differential diagnosis is essential to ensure the correct diagnosis and appropriate treatment. In some cases, Baxter’s nerve entrapment, a condition characterized by entrapment of the nerve in the heel area, may present with symptoms similar to plantar fasciitis.
MRI imaging plays a crucial role in distinguishing between these conditions, as it reveals soft tissue abnormalities and helps clinicians make an accurate differential diagnosis. It is important to consult with a healthcare professional for a comprehensive evaluation and correct diagnosis of heel pain.
Baxter’s Nerve Entrapment
Baxter’s nerve entrapment is a condition that involves the entrapment and compression of the nerves in the heel area, leading to heel pain. The symptoms of Baxter’s nerve entrapment can mimic those of plantar fasciitis, making it challenging to differentiate between the two.
MRI imaging is instrumental in the differential diagnosis of Baxter’s nerve entrapment and plantar fasciitis. The detailed soft tissue images obtained from an MRI scan allow for the identification of abnormalities, such as nerve entrapment or inflammation, assisting clinicians in accurately diagnosing the condition and providing appropriate treatment.
Heel Pain Etiologies
Heel pain can have various etiologies, and diagnosing the correct cause is essential for effective management. Plantar fasciitis, retrocalcaneal bursitis, tarsal tunnel syndrome, and calcaneal apophysitis are a few conditions that can cause heel pain.
Differential diagnosis plays a crucial role in distinguishing between these conditions, as their symptoms can overlap. MRI imaging, such as plantar fasciitis MRI scans, aids clinicians in evaluating the soft tissue abnormalities associated with these conditions.
By examining the detailed images provided by the MRI, clinicians can accurately diagnose the cause of heel pain and recommend the appropriate treatment for each specific condition.
Interpretation of MRI Results
Interpreting the results of an MRI scan for plantar fasciitis requires a specialized radiologist, trained in the interpretation of musculoskeletal imaging. The radiologist analyzes the signal intensity of the plantar fascia, looking for abnormalities such as high signal intensity, inflammation, thickening, or rupture.
These findings, combined with clinical history, physical examination, and other diagnostic tests, aid in the diagnosis of plantar fasciitis. The radiology report provides detailed descriptions of the MRI findings, helping healthcare providers guide the appropriate treatment plan for each individual patient.
Normal Results
When the MRI scan of the plantar fascia shows normal results, it indicates the absence of abnormalities, inflammation, swelling, or rupture. Normal plantar fascia images will exhibit low signal intensity, suggesting the healthy state of the plantar fascia. This finding helps clinicians rule out plantar fasciitis and consider other potential causes of heel pain.
However, it’s important to note that the diagnosis of plantar fasciitis relies on a combination of clinical examination, patient history, and imaging results. If heel pain persists despite normal MRI results, further evaluation may be necessary to determine the cause of the symptoms.
Abnormal Results
In cases where the MRI scan reveals abnormalities, such as high signal intensity, inflammation, or thickening of the plantar fascia, clinicians can confirm the diagnosis of plantar fasciitis. These abnormal findings are indicative of severe plantar fasciitis, which may require additional treatment interventions.
The radiologist will also assess the extent of inflammation, the presence of edema, and the potential rupture of the plantar fascia, providing crucial information for the treatment planning process. The radiology report, along with other clinical findings, guides healthcare providers in developing an appropriate treatment plan, tailored to the individual patient.

Treatment Options Based on MRI Results
The treatment options for plantar fasciitis are influenced by the MRI results. Non-surgical treatments, such as stretching exercises, physical therapy, orthotics, and anti-inflammatory medications, are typically recommended for milder cases of plantar fasciitis. However, severe plantar fasciitis, diagnosed through abnormal MRI results, may require more aggressive treatment, such as corticosteroid injections or extracorporeal shockwave therapy.
Surgical interventions, such as plantar fascia release, are reserved for cases of chronic plantar fasciitis or cases that do not respond to non-surgical treatments. The MRI results provide valuable insights for healthcare providers in determining the most appropriate treatment approach for each individual patient.
Non-surgical Treatments
Non-surgical treatments are usually the first line of defense for plantar fasciitis. These treatments aim to relieve pain, reduce inflammation, and promote the healing of the plantar fascia. They can include:
- Stretching exercises: Stretching the calf muscles and the plantar fascia itself can help alleviate pain and improve flexibility.
- Physical therapy: A physical therapist can guide patients through exercises, stretches, and techniques to strengthen the foot and ankle, reduce pain, and improve function.
- Orthotic devices: Custom orthotic inserts, arch supports, or night splints may be recommended to provide support and alignment, reducing stress on the plantar fascia.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Medications such as ibuprofen or naproxen can help reduce pain and inflammation associated with plantar fasciitis.

Surgical Treatments
Surgical treatments for plantar fasciitis are typically reserved for severe cases or cases that do not respond to non-surgical interventions. Surgical options include:
- Plantar fascia release: This procedure involves partially or completely releasing the plantar fascia from the heel bone, relieving tension and reducing pain. It can be performed using minimally invasive techniques or open surgery, depending on the severity of the condition.
- Tenex procedure: The Tenex procedure is a minimally invasive technique that uses ultrasound imaging to guide the removal of damaged tissue in the plantar fascia, promoting healing and pain relief.
- Gastrocnemius recession: In cases where tight calf muscles contribute to plantar fasciitis, the gastrocnemius muscle may be lengthened surgically, allowing the foot to move more freely and reducing stress on the plantar fascia.
- Surgical treatments for plantar fasciitis are typically considered after conservative measures have been exhausted, and the symptoms persist or worsen. Your healthcare provider will consider the MRI results, clinical findings, and your specific circumstances to determine the most appropriate course of treatment.
Long-term Management and Prevention of Plantar Fasciitis
Once diagnosed with plantar fasciitis, long-term management and prevention strategies are crucial to minimize the risk of recurrence. These strategies may include:
- Continuation of stretching exercises and physical therapy to maintain foot and ankle flexibility and strength.
- Wearing supportive, well-fitting shoes with adequate arch support and cushioning.
- Avoiding high-impact activities or prolonged standing on hard surfaces.
- Gradual return to physical activities, such as running, after a period of rest and rehabilitation.
- Regular follow-up with healthcare providers for ongoing monitoring of the condition and adjustment of the treatment plan, if necessary.
How can an MRI Scan guide long-term care for Plantar Fasciitis?
An MRI scan for plantar fasciitis plays a crucial role in guiding long-term care for the condition. By evaluating the extent of inflammation, swelling, or rupture of the plantar fascia, the MRI scan provides valuable information for treatment planning and ongoing management. The scan helps healthcare providers assess the severity of the condition, determine the most appropriate treatment options, and monitor the progress of the treatment plan over time.
The detailed images obtained from the MRI scan allow for the identification of subtle changes, such as the resolution of inflammation or the healing of the plantar fascia, guiding clinicians in adjusting long-term care strategies for plantar fasciitis patients.
The MRI scan can provide a baseline for comparison to future scans, helping healthcare providers track the efficacy of treatment interventions and make informed decisions about the long-term care of plantar fasciitis patients.
How accurate is an MRI for diagnosing plantar fasciitis?
MRI scans are considered highly accurate for diagnosing plantar fasciitis. They provide detailed images of the soft tissue structures, revealing abnormalities, inflammation, swelling, or rupture of the plantar fascia. MRI imaging offers a comprehensive evaluation of the foot, allowing for an accurate diagnosis and differentiation from other conditions that may present similar symptoms.
However, it’s important to note that the diagnosis of plantar fasciitis relies on a combination of clinical examination, patient history, and imaging results, and the expertise of the healthcare provider. If symptoms persist despite normal MRI results, further evaluation may be necessary to determine the cause of the pain.
Are there any risks associated with getting an MRI for plantar fasciitis?
MRI scans for plantar fasciitis are generally safe and non-invasive. However, there are some considerations and potential risks to be aware of. Magnetic resonance imaging utilizes a strong magnetic field and radio waves, which can interfere with certain metal objects, such as pacemakers, cochlear implants, or metal implants. It’s vital to inform the imaging facility of any medical conditions or the presence of metal implants before the scan. T
here is also a small risk of an allergic reaction to the contrast dye used in some cases, although this is rare. The contrast dye can help enhance the imaging of soft tissue abnormalities, but it’s not always necessary for plantar fasciitis imaging. As with any medical procedure, it’s crucial to discuss any concerns or potential risks with your healthcare provider before undergoing an MRI scan.
Conclusion
Living with plantar fasciitis can feel like an uphill battle, but it’s one you don’t have to fight alone. The precision of MRI scans opens the door to customized treatment strategies, illuminating the path to relief. Coupled with the supportive resources and expert reviews available at TheHeelGP.com, sufferers have a comprehensive toolkit at their disposal to tackle plantar fasciitis head-on.
As we reflect on the journey from diagnosis to recovery, one question remains: What step will you take today towards reclaiming your stride?
I hope you found this blog helpful and please feel free to comment and share.
Thanks for reading!
 | Tracy J. Founder, The heel GP |