In the quiet moments before dawn, as the world lies still, there’s a story unfolding in homes around the globe. It’s not one of peace or restful sleep, but of individuals bracing themselves for the first steps out of bed, steps that are often met with a sharp, stabbing pain at the bottom of the foot. This is the daily reality for those battling plantar fasciitis, a condition that turns the simple act of walking into a formidable challenge. Amidst this struggle lies a beacon of hope: the journey to relief begins with a proper diagnosis, and at the heart of this diagnosis is the plantar fascia test.
Understanding Plantar Fasciitis
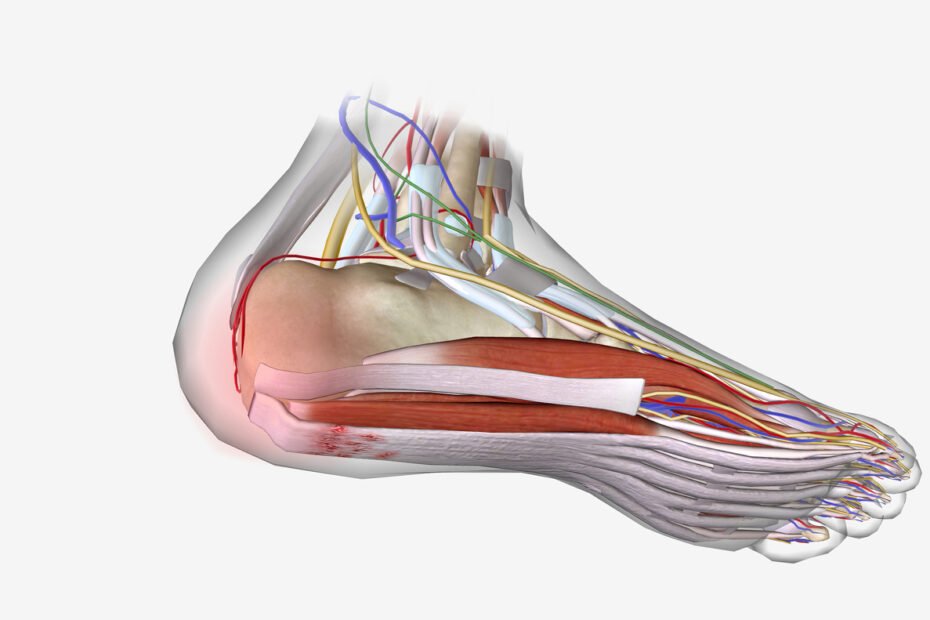
Plantar fasciitis is an inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of the foot and connects the heel bone to the toes. This condition is one of the most common causes of heel pain, especially in the morning when taking the first steps.
The pain can decrease throughout the day but may worsen after prolonged standing or physical activity. Ignoring the symptoms of plantar fasciitis can lead to chronic heel pain and limitations in daily activities. Understanding the causes of heel pain, including plantar fasciitis, is crucial for proper diagnosis and treatment.

Symptoms of Plantar Fasciitis
The primary symptom of plantar fasciitis is heel pain, particularly during the first steps in the morning or after a period of rest. The pain is usually described as sharp and located at the bottom of the heel. It can also radiate along the arch of the foot.
Other symptoms of plantar fasciitis may include:
- Increased pain after prolonged standing or physical activity
- Pain that improves with rest or limited weight-bearing
- Swelling and tenderness in the heel area
- Discomfort when walking barefoot or on hard surfaces
- It is important to seek medical attention if you experience persistent or worsening heel pain. A healthcare provider can perform a thorough examination, including a plantar fasciitis diagnosis test, to determine the cause of the pain and develop an appropriate treatment plan.

Risk Factors for Plantar Fasciitis
Several risk factors increase the likelihood of developing plantar fasciitis. Understanding these factors can help individuals take preventive measures and reduce the risk of developing this condition.
Common Risk Factors
While plantar fasciitis can occur in anyone, certain factors may increase the risk of developing the condition. Some common risk factors for plantar fasciitis include:
- Age: Plantar fasciitis is more common in middle-aged individuals, typically between the ages of 40 and 60.
- Obesity: Excess body weight adds stress to the plantar fascia, increasing the risk of inflammation and heel pain.
- Physical Activity: Engaging in activities that require prolonged standing, walking, or running can strain the plantar fascia, leading to its inflammation.
- Foot Mechanics: Structural abnormalities of the foot, such as flat feet or high arches, can alter foot mechanics and increase the risk of plantar fasciitis.
- Improper Footwear: Wearing unsupportive shoes or sudden changes in exercise intensity, such as switching from flat shoes to high heels, can contribute to plantar fasciitis.
- By identifying and addressing these risk factors, individuals can take preventive measures to reduce the likelihood of developing plantar fasciitis.
The First Step: Clinical Examination
A clinical examination is typically the first approach in diagnosing plantar fasciitis. During this exam, a healthcare provider will review the patient’s medical history and perform a physical examination of the foot. Key indicators of plantar fasciitis include pain in the bottom of the foot near the heel, especially notable with the first steps in the morning or after periods of rest.
Advanced Diagnostic Techniques
While a clinical examination can strongly suggest plantar fasciitis, further diagnostic tests might be necessary to rule out other conditions. Techniques such as ultrasound imaging and MRI (Magnetic Resonance Imaging) are used to visualize the plantar fascia and assess its thickness and any signs of inflammation or tears. Ultrasound, in particular, is beneficial for its ability to provide real-time images of the fascia, offering a detailed view of the condition’s impact.
The Role of the Plantar Fascia Test
The plantar fascia test, also known as the “windlass test,” is a simple yet effective diagnostic tool. The test involves flexing the toes upward while examining the foot’s arch and the plantar fascia’s response. A positive test—indicated by pain or discomfort in the arch or heel—can confirm the presence of plantar fasciitis. This test, combined with the patient’s history and other examination findings, plays a crucial role in diagnosing the condition.
Interpreting Plantar Fascia Test Results
Analyzing the outcomes of the plantar fascia test requires specialized knowledge. Healthcare providers use these results to validate the diagnosis accurately. The interpretation of the test findings is crucial in determining the most suitable treatments for the condition. This process involves connecting the symptoms experienced by the individual with the diagnostic test outcomes.
Precise interpretation of the test results plays a pivotal role in devising an effective plan for treatment, ensuring that the individual receives the most appropriate care.
Treatment Options for Plantar Fasciitis
Conservative treatments for plantar fasciitis aim to alleviate foot pain and promote healing. They often include physical therapy focused on the mechanics of the foot, strengthening exercises, and stretching routines to address the pain and improve function.
In cases where nonsurgical treatment is ineffective, more advanced options like extracorporeal shock wave therapy can be considered for pain relief, specifically for chronic plantar fasciitis. Furthermore, recalcitrant plantar fasciitis may require endoscopic plantar fasciotomy to release the plantar fascia tension and provide long-term relief.
Patients with chronic plantar heel pain or plantar fasciitis pain may benefit from these interventions, especially when other conservative measures have not been successful in managing the condition.
Conservative Treatments
Utilizing conservative measures for plantar fasciitis involves a combination of strategies to manage the discomfort effectively. These methods encompass rest, ice application, specific stretching exercises, and the utilization of supportive orthotic devices.
Physical therapy emerges as a pivotal component in the non-invasive management of plantar fasciitis, aiding in strengthening and flexibility enhancement. Night splints offer a non-surgical approach to alleviate heel pain by maintaining a prolonged stretch on the plantar fascia during sleep.
Lifestyle modifications, such as appropriate footwear choices and weight management, synergistically support conservative treatment plans aimed at symptom relief without resorting to surgical interventions.
How Effective is Extracorporeal Shock Wave Therapy?
Extracorporeal Shock Wave Therapy demonstrates potential for plantar fasciitis treatment. By targeting inflammation with shock waves, ESWT aims to heal and alleviate pain. Effectiveness varies per individual; consulting a healthcare provider is crucial for understanding benefits and risks.
Finding Relief: How TheHeelGP.com Can Help
For those navigating the challenges of plantar fasciitis, finding reliable and effective treatment options is crucial. TheHeelGP.com stands as a trusted resource, offering comprehensive reviews of treatment options tailored to those suffering from this condition. From physical therapy exercises and orthotic devices to more advanced treatments like shock wave therapy, we provide valuable insights to help sufferers make informed decisions about their care.
Can the plantar fascia test be painful?
The discomfort during the plantar fascia test may cause some discomfort but is not usually excessively painful. This diagnostic procedure involves assessing tenderness and inflammation by pressing on the plantar fascia. Brief discomfort is expected, informing your healthcare provider of significant pain is advisable.
What are the risks associated with undergoing a plantar fascia test?
Potential risks linked to the plantar fascia test are minimal, with slight discomfort or pain during the procedure being the primary concerns. Rare instances may involve risks of infection or bleeding, emphasizing the importance of adhering to post-procedure care instructions.
How accurate is the plantar fascia test in diagnosing plantar fasciitis?
The plantar fascia test proves reliable for diagnosing plantar fasciitis, involving pressure on the plantar fascia to elicit pain. A positive result signifies inflammation and microtears. Combining this test with imaging studies like ultrasound or MRI can enhance its accuracy.
Can the results of a plantar fascia test indicate any other foot conditions besides plantar fasciitis?
The outcomes of a plantar fascia test may reveal other foot issues like heel spurs, Achilles tendonitis, or stress fractures. While sharing similar symptoms with plantar fasciitis, these conditions require distinct treatment approaches for effective recovery. Seeking professional help for accurate diagnosis and personalized treatments is paramount.
Conclusion
The journey through plantar fasciitis is marked by pain, frustration, and the relentless pursuit of relief. Yet, through proper diagnosis and tailored treatment plans, recovery is within reach. The plantar fascia test serves as a gateway to understanding and addressing the condition, offering a path out of the shadows of pain. As sufferers take the first steps towards recovery, supported by resources like TheHeelGP.com, the question remains: What change will your first pain-free step bring?
I hope you have found this blog helpful and please feel free to comment and share.
Thanks for reading!
 | Tracy J. Founder, The heel GP |