Introduction
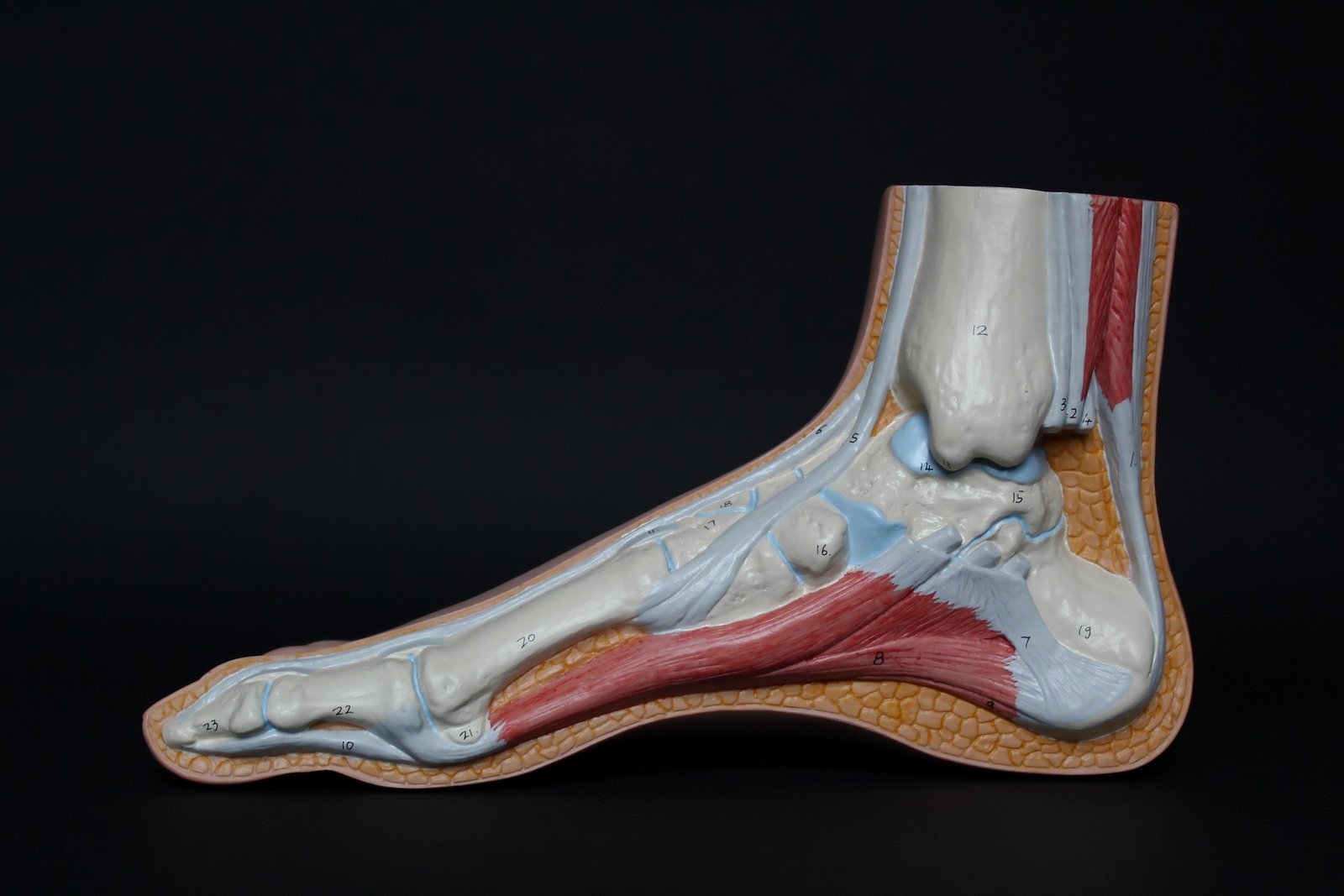
What about plantar fasciitis? Well, it is a common foot condition which around 1 in 10 people suffer from. It is characterised by inflammation of the plantar fasciitis. This is a thick band of tissue that runs along the bottom of the foot.
So, let’s explore the history of the condition, causes, symptoms and diagnosis and hopefully this will answer the question!
History
Ancient Times
- It is believed that the condition has likely existed for centuries, although historical records of its diagnosis and treatment are understandably limited.
- You would have expected that some ancient cultures, for example the Egyptians, might have recognised similar foot conditions.
19th Century
- Wood in 1812 first described plantar fasciitis and attributed it to tuberculosis.
- Plantar fasciitis was previously referred to as ‘policeman’s heel’ and ‘runner or joggers heel’ as it appeared to be associated with that sport and profession. However, the term ‘plantar fasciitis’ eventually emerged in the 19th century.
20th Century
- The medical profession’s understanding of plantar fasciitis improved during the 20th century.
- This was due to the improvements in radiology and orthopedics.
- X-rays really helped in visualising the condition, and treatments at that time included rest, stretching exercises and a variety of orthotic devices.
Late 20th Century
- A number of non-surgical treatments became available.
- These included, physical therapy, custom orthotics, and corticosteroid injections.
- Extracorporeal shockwave therapy (ESWT) has also emerged as an alternative treatment option.
21st Century
- Plantar fasciitis continued to be a prevalent condition.
- This is especially prevalent among athletes and individuals with flat feet or high arches.
- Treatments have expanded to include newer methods like platelet-rich plasma (PRP) injections and minimally invasive procedures.
Plantar Fasciitis Causes
This foot condition is typically caused by excessive strain on the plantar fascia, which is a band of tissue that connects the heel bone to the toes. Some common causes and risk factors include:
- Overuse: Repeated stress and strain on the feet, often from activities like running, walking, or standing for extended periods. Some people may not be able to control this overuse, particularly if it is connected to their employment.
- Poor Foot Mechanics: Some individuals have, through no fault of their own, have abnormal foot arches (flat feet or high arches). This can put extra stress on the plantar fascia.
- Unsuitable Footwear: If you wear shoes with inadequate arch support or poor cushioning, then this can contribute to plantar fasciitis.
- Obesity: Carrying excessive body weight increases the load on the plantar fascia. Thus, increasing the risk of inflammation and pain. It can be challenging, but even some weight loss can make a difference.
- Age: Plantar fasciitis is more common among people between the ages of 40 and 60. As stated earlier, plantar fasciitis affects about one in every 10 people. But the statistics are significantly higher for the elderly and older adults.
- Tight Calf Muscles: Tightness in the calf muscles can lead to increased stress on the plantar fascia. When the calf muscles are too tight, the ankle can’t really bend far enough. This results in the strain of the calf muscles onto the heel bone and then into the attachment from the heel bone into the plantar fascia.
- Rapid Changes in Activity: Sudden increases in activity levels or changes in exercise routines can strain the plantar fascia. It may be that you need to improve your load tolerance first, before embarking on an increased activity level.
- Occupational Factors: Jobs that involve prolonged standing or walking on hard surfaces may increase the risk. This is particularly true for retail and hospitality sector staff.
- Biomechanical Issues: Issues with gait or walking mechanics can lead to higher than normal levels of stress on the plantar fascia.
It’s important to recognise that while these are common causes and risk factors, the exact cause of plantar fasciitis can vary from person to person. Proper diagnosis and treatment by a healthcare professional is imperative for managing this condition.

Symptoms of Plantar Fasciitis
Plantar fasciitis typically causes symptoms such as:
- Heel Pain: This is the most common symptom. It is often a sharp, stabbing pain in the heel, usually near the front and bottom.
- Foot Arch Pain: Pain or discomfort in the arch of the foot.
- Stiffness: Stiffness and discomfort in the morning, which may improve with movement.
- Pain with Activity: Pain that worsens with prolonged standing, walking, running, or after sitting for a while.
- Tenderness: The affected area may be tender to touch.
- Swelling: Some people may experience mild swelling in the heel area.
- Difficulty Walking: Pain may make it difficult to walk or stand for extended periods.

Diagnosing Plantar Fasciitis
According to the National Institute for Health Care Excellence (NICE)(2020)
Plantar fasciitis is usually diagnosed by the history and physical examination findings alone.
- Ask about the nature of the heel pain, and the general health and physical activity of the person.
- Characteristic symptoms of plantar fasciitis include:
- An initial insidious onset of heel pain.
- Intense heel pain during the first steps after waking or after a period of inactivity, with relief upon initiation of movement.
- Pain that reduces with moderate activity, but worsens later during the day or after long periods of standing or walking.
- Characteristic symptoms of plantar fasciitis include:
- Document any risk factors, such as age between 40–60 years, overweight or obesity, running, or prolonged standing or walking.
- Examine the foot at rest (when sitting) and when standing and walking. Signs of plantar fasciitis include:
- Tenderness on palpation of the plantar heel area (particularly, but not always, localized around the medial calcaneal tuberosity).
- Limited ankle dorsiflexion range (with the knee in extension).
- Positive ‘Windlass test’ (reproduction of pain by extension of the first metatarsophalangeal joint).
- Tightness of the Achilles tendon.
- An antalgic gait (abnormal walking to avoid pain) or limping.
- If clinical features of plantar fasciitis are absent or inconsistent, consider an alternative diagnosis.
- If the diagnosis is uncertain, referral to a podiatrist or orthopaedic surgeon for further investigation (depending on the suspicion of the cause) may be necessary.

Summary – What About Plantar Fasciitis?
Plantar Fasciitis is believed to have been present in ancient times, however, the first evidence of the condition being formally recognised was by Wood in 1812.
Plantar Fasciitis continues to be a prevalent condition in modern society. It is estimated that 1 in 10 people suffer from this condition at any one time.
There are common symptoms and risk factors associated with this condition. Some symptoms we don’t have control over, but some we do.
Plantar fasciitis can be an extremely painful condition at times, particularly when you get up for the first time in the morning! It can be debilitating and frustrating, but it can be managed and overcome.
Should you find that you have sharp pain in your heel, and this has lasted for more than a few weeks, then the first step is to make sure you go to your General Practitioner/ Health Professional for diagnosis.
Once diagnosed there are plenty of treatment options which can help manage or eradicate this painful condition.
In future blogs, I will be examining the best treatment options for plantar fasciitis. So, please check them out at my website https://theheelgp.com
Can’t find what you are looking for? Then please contact me and I will try and help.
Thanks for reading and I hope you find this article helpful.
 | Tracy J. Founder, The heel GP |